A complete guide to PIRP notes (with example)
Clinical documentation is an essential part of every therapist’s job.
Each session must be documented for legal, insurance, and clinical purposes to protect both client and therapist.
In this article, we’ll explore what PIRP notes are, when to use them, and how to write them. We’ll also share a PIRP note example from Grace Meyer on our Clinical team.
If you’re a little unsure about which progress notes to use, we recommend starting with our article comparing some of the most popular progress notes available.
And finally, we’ll provide a PIRP template that you can download for free.
What is a PIRP note?
PIRP notes are a progress note type used by mental health professionals such as psychotherapists, counselors, social workers, psychiatrists, and psychologists.
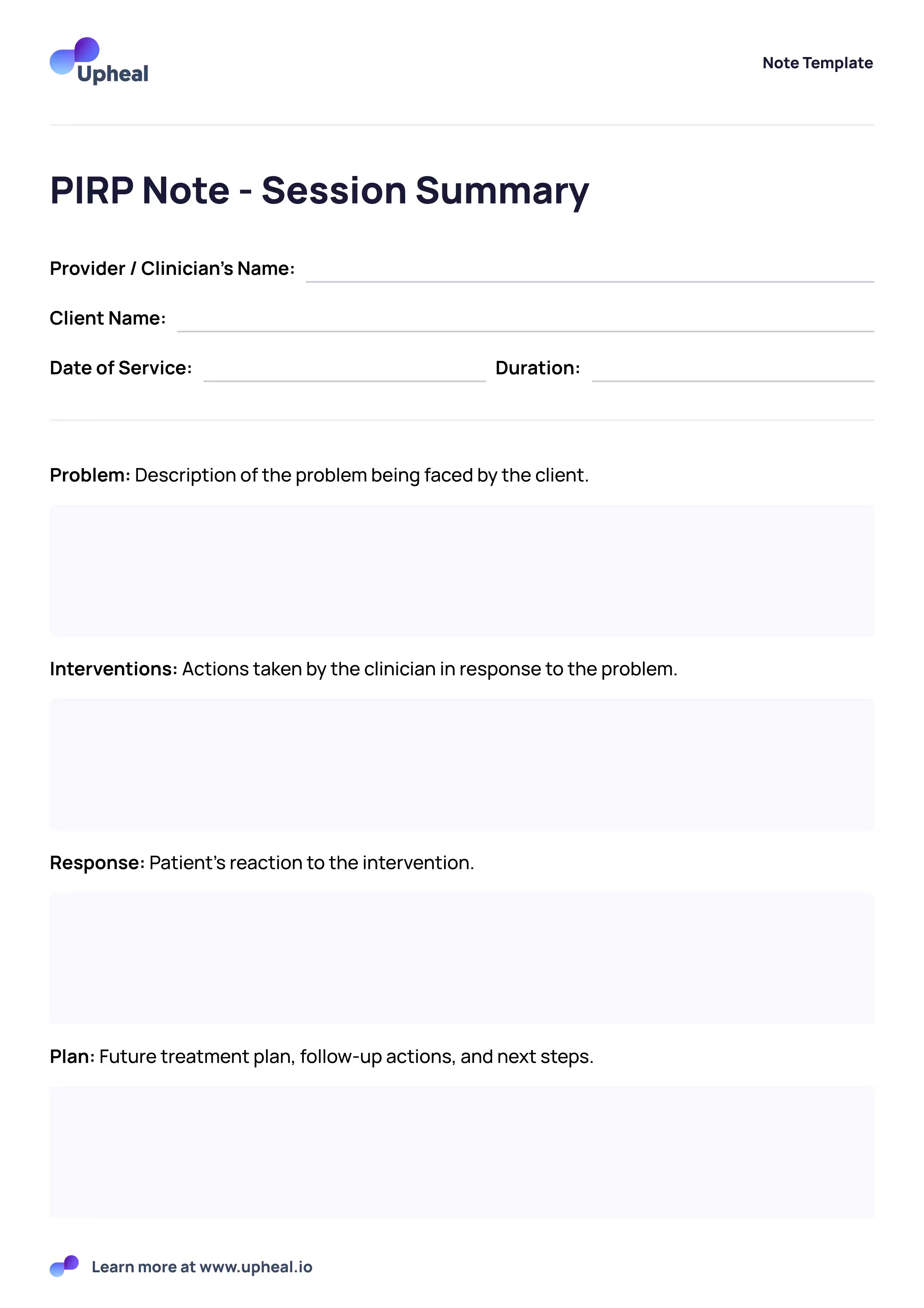
The PIRP note acronym stands for Problem, Intervention, Response, and Plan. Each of these sections is an essential component of the mental health PIRP note a practitioner has to write when using this particular note format.
The PIRP note components:
- Problem (P): Describes the problem being faced by the client.
- Interventions (I): Actions taken by the clinician in response to the behavior.
- Response (R): Patient's reaction to the intervention.
- Plan (P): Future treatment plan, follow-up actions, and next steps.
Writing notes in a PIRP format offers a structured picture of the client’s problem and their progress toward resolving it.
The PIRP note – a real-world scenario
Jeff Kashou, therapist and our Senior Clinical Product Lead, has picked the following scenario that’s well-suited to PIRP notes from his years in therapy practice.
The therapist will describe the problem first, capturing the client’s current difficulties.
They will then choose the most relevant interventions, in this case, psycho-education on the self-harm cycle, emotional regulation, and distress tolerance strategies, as well as a brief look at underlying triggers and cognitive distortions contributing to self-harm urges.
In the response section, the therapist will then capture the client’s thoughts and feelings that arose as a result of the interventions, such as the client being able to identify specific steps they would take in moments of distress, feeling less out of control, and more regulated by the end of the session.
In the plan section, the therapist documents any agreed-upon strategies, such as tracking self-harm urges and keeping a thought log or practicing at least one distress tolerance skill, as well as what will be addressed in the next session.
Patient PIRP note example – written by a therapist
3 important benefits of the PIRP note template
Using the PIRP note template allows for heightened focus on a particular problem. This makes the PIRP note well-suited to more serious issues, such as self-harm, severe depression, and more.
- Highly problem-focused: PIRP notes are excellent at focusing on a particular client problem. This can range from managing the effects of neurodivergence to dealing with self-harm behaviors. The PIRP notes document the client's presenting problem in great detail, ensuring the clarity and specificity needed for a very targeted treatment approach.
- Allow for easy re-evaluation of progress: Using PIRP notes allows the focus of treatment to be evaluated and adjusted as needed so that precious time isn’t wasted on interventions that aren’t working. When using a mental health PIRP note, there is significant emphasis on the client's response to various interventions used, making tracking changes easy and flexible.
- Good for crisis intervention: PIRP notes are effective at crisis intervention because they specifically hone in on the problem or set of problematic behaviors the client is experiencing. The PIRP format structure allows you to remain organized and focused, ensuring that all necessary information is captured and any follow-up plans, referrals, or additional services are recorded.
PIRP note template pdf
Use our free PIRP note template for your client sessions – it’s free to download.
How to write a PIRP note – a step-by-step guide
Here’s our head therapist’s step-by-step guide using the PIRP acronym.💡 It’s a neat way to remember what you’re trying to capture in each section.
Your PIRP notes cheat sheet – the sections step by step
Here’s how to remember and understand PIRP sections in 4 easy steps.
- P: What is the problem the client is facing? What are the physical and emotional aspects?
- I: How did I, the therapist, intervene? What did I do to help the client with their situation?
- R: What was the client’s response to that? How well did it work or not? How did they feel?
- P: What’s the plan going forward in the next session(s)?
Common use cases for the PIRP note template
1. Crisis intervention
PIRP notes work well in situations requiring fast and precise documentation, such as crisis intervention or short-term therapy. Their structured format ensures that immediate concerns are addressed with clarity, making them particularly helpful in urgent therapeutic settings.
2. Shorter-term therapy
Since PIRP notes get right at the issue fast, they’re a great choice for when you know you have a specific issue to treat in a limited timeframe. In addition, they can be shared with other practitioners when you are working in a multidisciplinary team and only get to see a client for a few sessions, enhancing continuity of care.
3. Added compliance and accountability
Well-documented PIRP notes serve as legal protection for therapists, demonstrating adherence to ethical and legal standards, and supporting compliance with regulatory and insurance requirements.
4. Private practice or organization
Whether you work for yourself or in a larger organization, PIRP notes give a clear, organized format for documenting important aspects of therapy sessions, ensuring consistency and completeness across multiple sessions and providers, providing a shared understanding of a client's treatment plan and progress.
6 tips for writing excellent PIRP notes
- Be clear and specific: State the problem and or diagnosis concisely. Stay objective, avoiding personal judgements, or interpretations.
- Include additional, measurable context: Capture the duration and intensity of symptoms and previous treatments or conditions affecting the client’s experience.
- Capture the client’s perspective: Use quotes and include the client’s interpretations.
- Consider comorbidities: If there are interconnected medical conditions, add them to the problem statement. Describe the relationship to create a holistic understanding.
- Avoid jargon and acronyms: Use standardized terminology. Your shorthand won’t be familiar to all healthcare professionals, so it’s best to stick to terms everyone will know.
- Be timely: Writing your notes promptly makes all the difference when it comes to clinical accuracy, relevance, and insights. Try to do so within 48 hours, or have them done almost instantly with an AI note-taking tool like Upheal.
- Review changes over time: Make sure to review the client’s growth from a longer-term perspective, reflecting on their journey and challenges to arrive at new treatment ideas or simply celebrate the client’s growth.
Additional insights
Although clinical documentation is necessary, it doesn’t necessarily need to be time-consuming. Using a trustworthy automated platform like Upheal can speed up the process greatly.
And it’s not just about the speed – although saving you time for yourself or other clients is absolutely something we strive for, we’re keen to also support various aspects of psychotherapy to empower and support clinician’s in their work as much as possible.
Take a look at our AI-powered PIRP note.
A draft is created for you, allowing you to save time by simply reviewing and editing, rather than writing an entire session note from scratch.
Concluding thoughts
Now that you know all about the PIRP note, you can use it when and if you come across some of the cases and situations described above.
As we explored, the PIRP note is the perfect choice for providing a good balance of internal and external landscapes, and allows you to be treatment and intervention focused, while still spending time on the client’s internal state and assessment.
Of course, each clinician is free to use whatever progress note style they prefer. However, it’s our experience that clinicians are incredibly busy out of the gate, and some aren’t taught documentation at university! Hopefully, you’ll now have an idea of what the PIRP note is all about, and when appropriate add it to your admin routine and therapeutic care.
Happy writing!