Suicide Prevention Month: Why mental health professionals may be at more risk than their clients

Mental health professionals are often involved as ‘gatekeepers’ in the management of suicidality and suicide prevention.
For the sake of our mission and our audience, we wanted to dive into this topic, not from the perspective of the client, family member, friend, or colleague (though some of us have written about that privately too) – but rather from the perspective of the clinician who may be trying to stay afloat. Who is over and over, exposed to those at crisis point.
In the same way that a surgeon has a patient’s life in their hands, so too does a psychotherapist, psychiatrist, or clinical psychologist. A high-pressure, high-risk job that involves persistent discourse in managing the psychological distress of others.
Where clients can leave a therapy session or medical office (hopefully) with a sense of relief and healing, MHPs are left to move on to the next client with not a lot of time in between. In this article, we’ll explore a whole range of risk factors to look out for.
With enough preparation, knowledge, and validation of the difficulties involved in being an MHP, we can find new means of support.
Are MHPs really more at risk?
Contrary to what we may think, being an MHP does not make one immune to trauma, mental health challenges, or the natural nervous system responses that arise when working with distressed clients.
“Even before COVID-19, in a survey of 462 psychologists, 62% self-identified as depressed, and 42% reported some form of suicidal ideation or behavior.”
Due to the nature of their work, MHPs are exposed to emotional distress much more than the average person.
Although the research shows that all healthcare professionals are at elevated risk for suicide, of those in mental health, psychiatrists, clinical psychologists, and clinical social workers are most affected. (Corcoran, 2022; Banerjee 2020.)
When reviewing the research, we found 6 risk factors. Each is worthy of its own blog article, but what strikes us most, is the fact that MHPs are likely to be at risk for almost all of these.
- Burnout
- Vicarious trauma
- Own trauma background
- Empathy (and compassion fatigue)
- Stigma
- Readily available self-medication
Delving deeper – MHPs and burnout
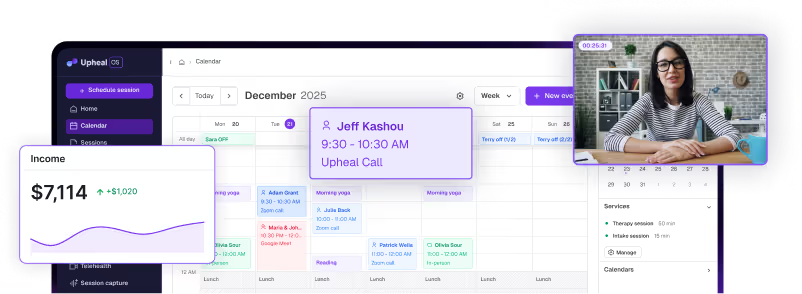
Among therapists, almost half report that they’re burned out (Lin et al., 2023) and it’s true; we’re less healthy mentally, so therapists have more and more clients with more and more serious issues. (At Upheal, we’re glad to be working to at least support the documentation part of the job.)
But burnout doesn’t just mean being overworked. Many factors can cause burnout: it’s been associated with workplace climate, caseload size, and severity of client symptoms (Acker, 2011; Craig & Sprang, 2010; Thompson et al., 2014) as well as practitioner empathy levels, trauma work, and working largely with clients that have personality disorders.
Overall, in the mental health provider sense, burnout is a complex loop different from the burnout of a project manager. It goes something like this:

The process of not being able to connect to patients fully on a deep emotional level has been called de-personalization.
As MHPs try to protect themselves, they also curb their ability to offer empathy to their clients, which affects treatment quality and their clients’ capacity to heal.
Unfortunately, compassion satisfaction is then affected, which has actually been shown to shield MHPs from the negative effects of trauma.
💙 On the positive side:
- When therapists get compassion satisfaction from the job, i.e. when they see they’re making a positive difference, this buffers the effects of burnout and trauma.
- Smaller caseloads, less paperwork, and more flexibility at work are associated with lower rates of burnout (Lent & Schwartz, 2012).
- Therapists who have more years of supervision seem to be less likely to confront burnout. (Iosim et al., 2022; Koukenou, 2023).
- Keeping yourself regulated and well (physically, emotionally, and spiritually) can help you stay protected from stress and burnout.
💪 What to do:
It might seem as though mental health professionals are expected to cope alone and regulate their emotions and themselves aboard a sinking ship so to speak, of larger systemic and societal issues. But isolation and silence don’t work!
It’s not easy to propose solutions to such large issues, but sharing regularly and vocally, about unrealistic caseloads and low pay in a challenging economic climate, and increasing demand for mental health services – is one way of drawing attention to problems so others can see them too.
And we must call attention to them.
On top of that, on an individual level, here are a few practical ways you can alleviate some of the stress:
- Create a diverse client list with both serious and easier cases.
- Save time using an AI platform for documentation like Upheal.
- Find or create a supportive community.
- Reduce your caseload to fit your emotional and financial requirements.
- Find work in a supportive environment that aligns with your values.
- Seek supervision when necessary and use the sessions to discuss coping strategies.
- Write a “Clients I’ve helped list’ to remind yourself of your capabilities.
- Care for your physical health: burnout can also mean headaches and gastrointestinal problems (Kim et al., 2011).
Vicarious trauma and empathy
Experiencing vicarious trauma has been found to be one of the highest work risks for therapists' mental health.
Clients who have experienced trauma can be consistently assailed with memories, images, sounds, and other painful recollections.
The MHP, in connecting with and empathetically engaging in the clients' trauma, can experience detailed narratives of assault, rape, debilitating illness, loss of loved ones, or accidents – which can make it feel as though they are experiencing it too.
And of course, in a day, the MHP may experience several different trauma narratives vicariously.
A note: working in certain sensitive areas like gender-based violence and childhood sexual abuse can trigger self-traumatization, similar experiences of the past, and childhood attachment patterns, which can further lead to maladaptive coping, stress, sleep disturbances, and depression: all of which can be risk factors for suicides (Coleman et al., 2018).
💙 On the positive side:
- The literature suggests that therapists experience growth and development alongside vicarious trauma by witnessing their clients’ resilience and growth.
- Trauma can be healed and the rise of more trauma-informed treatments means you can further heal or educate yourself.
💪 What to do:
- Care for your body and nervous system: try massage, exercise, nature.
- Work with your nervous system: sing, create, dance.
- Practice mindfulness: meditate and self-reflect, observe.
- Do breath-work for relaxation: working with your exhales.
- Go to your personal therapy: work through any unresolved issues.
- Eat well, sleep well, and reach out to your supportive connections.
A trauma background creates more trauma
According to the Trauma Research Foundation, MHPs often have their own trauma history, which is the reason they turn to the profession (a phenomenon known as The Wounded Healer).
However, this often means they also have a predisposition toward being more vulnerable to further trauma.
Even for those who have done their own healing, experiencing trauma could mean being left with a biological imprint that can become “reactivated” so to speak, when we re-experience difficult things. And whether that’s because of our affected amygdala, hippocampus, or nervous system, we’re just more at risk.
We know from trauma work, that if one bad thing happens, we get over it more easily than when we’re exposed to multiple adverse experiences (also known as complex trauma). Witnessing more and more difficult things, essentially means it’s harder and harder to cope and return to a “normal” baseline.
Complex trauma may be a recurrent component in the lives of many MHPs.
The intrinsic and extrinsic pressures of the profession, persistent discourse in managing the psychological distress of others, professional burnout, self-stigma, societal apathy, and easy access to psychotropics are certain factors that make MHPs more vulnerable. This disengagement and stress can contribute to depression, anxiety, and complex trauma in MHPs.
And as we know, those with depression are 20 times more likely to take their own life.
💙 On the positive side:
- Trauma can be healed and, mental health care is more trauma-informed these days, which means you can further heal or educate yourself.
- Depression can respond to spiritual and existential approaches more than medication. (Leung, 2023; Peselow et al.,2013)
- A good personal trauma therapist can do wonders to help you stay regulated and help process unresolved issues.
💪 What to do:
- Find your own trauma therapist, try EFT, and somatic experiencing.
- Make sure you take care of further depression, anxiety, and addiction issues.
- Since trauma often exists with somatic symptoms, care for hyperarousal states and any physiological ailments and difficulties.
- Try a combat sport and take effective action.
- Work with your nervous system: calm and nourish your body.
- Build up your sense of self and interception.
- Do breath-work for relaxation: working with your exhales.
- Go to your personal therapy: work through any unresolved issues.
- Eat well, sleep well, reach out to connections.
Stigma – what if sharing means losing your license?
There is still much stigma in the world about expressing our emotions and struggles. And for therapists, this becomes even more difficult.
For the MHP, stigma exists at three levels – self, societal, and professional. There are fears of personal inadequacy, i.e. being able to do the job, fears around societal perception, and that of the mental health community.
Admitting to challenges in the very field where we are supposed to be “experts” can bring a sense of failure.
As a result, seeking help for or even talking about mental health challenges is largely taboo, leading to worsening symptoms, including potential suicide attempts and jeopardized patient care. (Bridgeman & Galper, 2010)
Many mental (and medical) professionals worry that if they share their mental health disorders or challenges, they may be judged or shamed by colleagues and patients.
They might also have their privacy invaded, be investigated, and potentially face issues renewing or receiving their medical license. (Banerjee et al, 2020).
An online survey showed that of 80% of respondents reporting burnout, 20% were against seeking any sort of assistance or help (Bhugra et al., 2019) despite having a diagnosable psychiatric illness cross-sectionally or in the past 1 year (mainly depressive disorder and substance use disorder).
Furthermore, symptoms of psychiatric illness (depression, etc.) may result in fatigue – actually limiting clinicians’ physical and cognitive ability to ask for help.
And finally, certain MHPs can also self-medicate easily. In a survey of psychiatrists (Balon, 2007) it was found that around 43% would consider self-medication if depressed.
Using psychoactive substances is a slippery slope and substance abuse like alcohol addiction acts as a gateway to further deterioration. It is simply a way to keep suffering in silence; thereby avoiding the main issues without finding proper resolution and healing.
It should be noted that depressed medical professionals don’t talk about the mental effects of their profession either. Despite depression, anxiety, and post-traumatic stress disorder (PTSD) being on the rise, they are afraid of losing their medical license or oversimplification and self-diagnosis can hinder them from seeking further help.
🖤 What not to do:
- Know that this is a truly difficult challenge to face and change. On the positive side, new legislation means that MHPs receive more protection than before.
- Some are already calling for a systemic change in our approach and treatment of this vulnerable population as it suffers in silence (Davidson et al., 2020).
- A few brave souls are braving the stigma to share vulnerably about their experiences so you don’t have to feel alone! Here and here – there are more out there, too.
- In general, stigma is lessening in recent times. Everyone is more interested in mental health.
- Counter shame with facts! Remember that in general, health-related professionals from dentists to physicians, to nurses and vets, have a higher risk for suicide as it is (Li et al., 2022). You are not weak, incapable, or different.
Conclusion
It’s not just the stressful nature of the job or the increasing severity of client symptoms. Quite a few factors exist that leave the MHP at elevated risk for mental health challenges.
The MHP, in connecting with and empathetically engaging in repeated trauma stories, might find themselves burned out especially when more risk factors are present at once. Burnout, vicarious trauma, the clinician’s own trauma background, internal and external stigma, high empathy, too little supervision, and an authoritarian workplace can all create the conditions for suicidal ideation.
To make things worse, the MHPs’ fear of becoming stigmatized or even deemed unfit for work, means they often suffer in silence – reaching for self-medicating short-term strategies and continuing into burnout, instead of treating and sharing the mental health challenges that arise on the job.
We sincerely hope this can change on a systemic level by receiving the attention and awareness this topic deserves and will continue to offer support by providing a platform for voices who want to speak out about it on our blog, as well as by streamlining the clinician’s documentation process as much as possible.