BIRP vs. SOAP notes
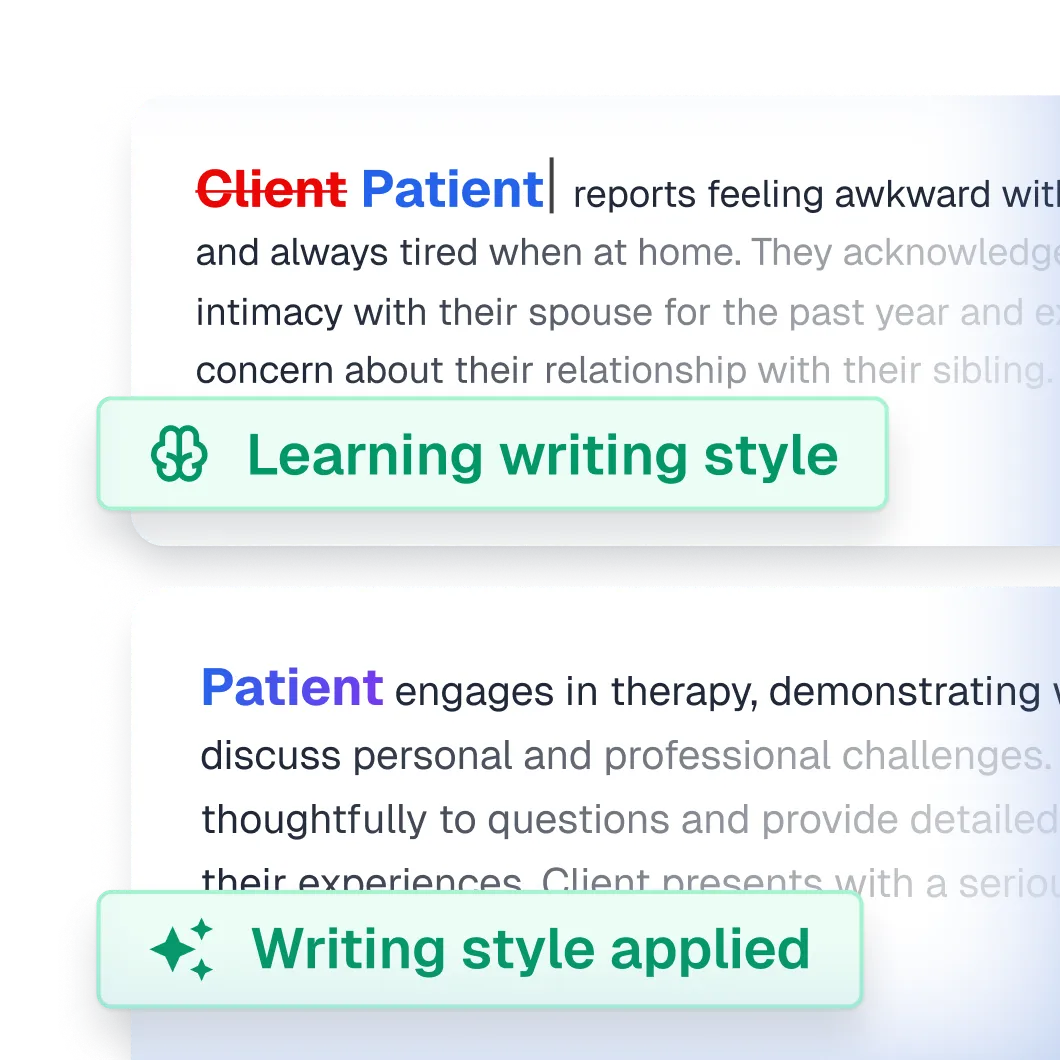
Therapists have a very demanding job to do in-session, and yet, they also have to stay on top of client documentation.
This means making sure that client progress is tracked using the aptly named (and legally required) progress notes.
Choosing the right documentation can help save time and better reflect both client and practitioner needs.
There are several different types of progress notes, but we’re going to focus on comparing BIRP vs. SOAP notes in this article.
If you’re not sure which to use, or simply always wondered about the difference between them, this article should help!
What is the difference between a SOAP note and a BIRP note?
Although both SOAP and BIRP notes are highly structured and have many benefits, they’re best suited to different scenarios.
Documenting sessions can be difficult and time-consuming (especially without Upheal ), but it does help; you, your client, and ultimately any healthcare professional who is involved with your client’s care.
While BIRP notes are focused on client behavior and used in behavioral health, SOAP notes are traditionally more comprehensive in their approach, with an emphasis on objective data and clinical assessment, and can be used in both medical and behavioral health settings.
We’ll compare both note types shortly, and take you through different scenarios for which note type to use and when. But first, let’s go through each note’s structure so can be used to reflect on (and evaluate) a client’s treatment plan.
The BIRP vs. SOAP note structure
BIRP notes – what are they?
The very focus of the BIRP note is client behavior; the first letter of the BIRP acronym.
While the BIRP note can be used in psychotherapy, psychiatry, and even group settings, it is most helpful for targeting behavioral health because it focuses on specific behaviors that the client is experiencing.
Behaviors such as drug addiction, skipping school, or overeating.
This can help clients learn how their thoughts and emotions influence their behavior. Over time, this can lead to new, more helpful coping strategies.
The BIRP note supports this focus on behavior-led treatment.
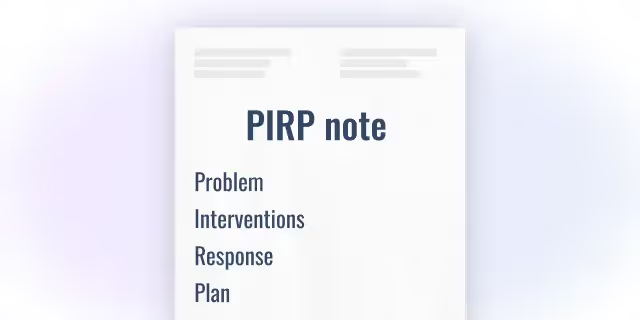
The BIRP note components
- Behavior (B): The client’s behavior, thoughts, and emotions; both observed and self-reported. This includes verbal and non-verbal cues including body language.
- Intervention (I): Actions taken by the clinician in response to the behavior. This can be any number of techniques, from mindfulness exercises to counseling techniques and more.
- Response (R): The client’s behavioral, cognitive, or emotional reaction to the intervention. This section is really important in evaluating the treatment's effectiveness.
- Plan (P): Future treatment plans, follow-up actions, and next steps based on the client’s response. It can include new interventions to try in future sessions or relevant client homework.
What is in a SOAP note?
SOAP notes are probably the most well-known and widely used progress note format.
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
While BIRP notes specifically focus on behavior, SOAP notes are more comprehensive and widely used in traditional healthcare and medical settings (like hospitals, nursing, physiotherapy, and more). They are also the most widely used note type in mental health care.
Overall, though the SOAP note can also measure client behavior, its focus is more on clinical outcomes and formal diagnosis.
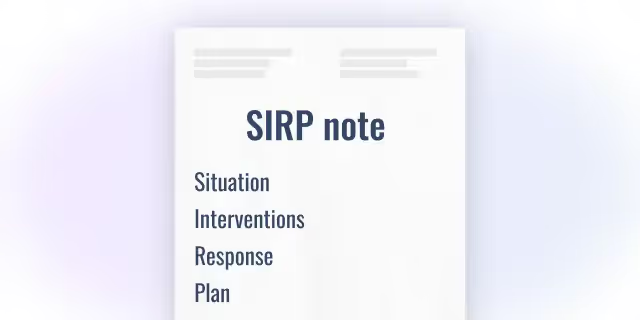
The SOAP note components
SOAP notes consist of four sections, splitting out self-reported and clinician-reported symptoms.
- Subjective (S): The patient's self-reported experiences, feelings, and concerns. For example, why they are presenting to therapy and their symptoms.
- Objective (O): Observable and measurable data collected by the clinician. This can be poor hygiene, an inability to focus, or slower response times.
- Assessment (A): The clinician's professional judgment and diagnosis based on the first two sections, as evidenced by symptoms described above, in this case, ones consistent with Major Depressive Disorder.
- Plan (P): The treatment plan, follow-up, and next steps, including client homework.
BIRP vs. SOAP – which note type to use when
In summary
Both note types succinctly capture client interactions in a standardized way, so that healthcare providers and insurance companies can easily understand clients’ unique treatment needs and history.
But as an overworked practitioner, every minute is precious.
Knowing the difference between BIRP and SOAP notes can help you capture and evaluate important clinical information in a way that’s well-suited to each patient’s treatment context and your specific needs as a clinician.
This can not only affect the client’s progress but also the time you spend writing and reviewing your notes. Therefore, your choice of notes needs to work for you!
While SOAP notes are especially helpful for documenting mental health symptoms such as mood, paranoia, anxiety, mania, and so on, using BIRP notes allows for greater focus on the behavioral symptoms and emotional responses, including their complex interplay.
This means BIRP notes are a great choice when treating addictions, eating disorders, self-harming behaviors (even ones in response to stress), and maladaptive coping behaviors in relationships.
That said, whichever format you choose, following each acronym helps standardize notes across sessions for greater focus when writing, the ability to compare progress over time, and contributes significantly to the quality of patient care and treatment planning.