How to write a DAP note – a real-life example
For mental health professionals, comprehensive yet succinct clinical documentation is key. The DAP progress note is an excellent way to capture client sessions and cover legal, insurance, and therapy-based requirements while tracking a client's progress.
In this article, we’ll walk you through DAP notes, how to write them, and when they might be the most helpful note type to choose.
Finally, we’ll provide a therapy DAP note example template that you can download for free.
What are DAP notes?
DAP notes are a form of progress note used by mental health professionals such as psychotherapists, counselors, psychiatrists, and other types of psychologists.
The mental health DAP note stands for Data, Assessment, and Plan. All of which the note must contain. However, unlike some other note types, a DAP note template is more flexible and tends to prioritize a deeper understanding of the client’s experience.
DAP note example
Here is an example from a real therapy scenario. How would you turn the following session into a mental health DAP note?
Below, you’ll see how our head of Head of Cinical Operations Ted Faneuff, (an experienced therapist), broke down a trauma-focused therapy session into each of the relevant DAP note sections.
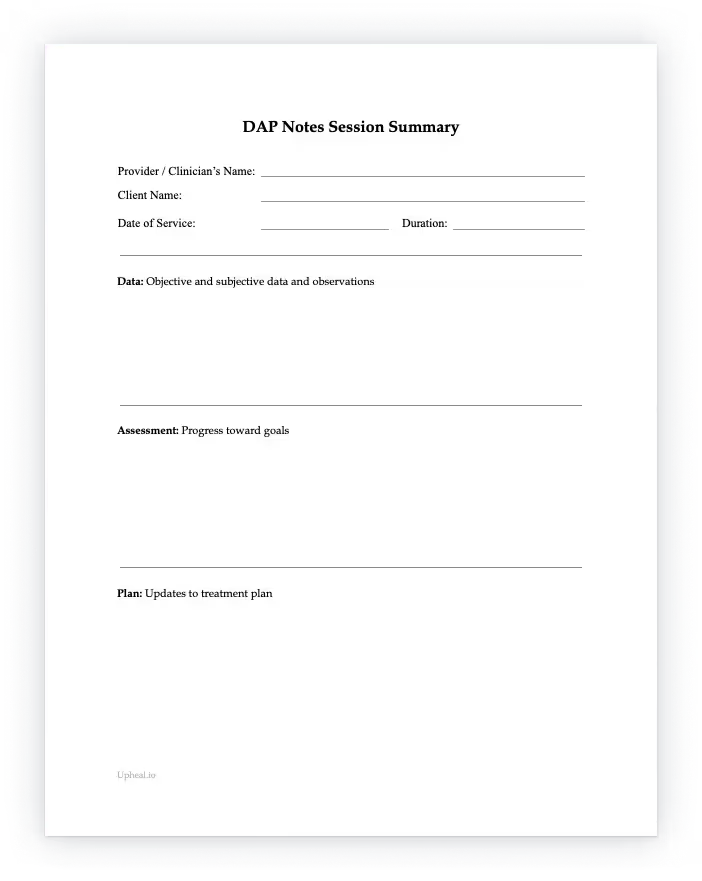
DAP note template pdf
Use our free DAP note template for your clients sessions – it’s free to download.
How to write a DAP note – a therapist’s DAP notes cheat sheet
In the example above, our Clinical Director looked for three important things about this session straight away.
These three sections are called the Data, Assessment, and Plan sections. If you’re writing a DAP note, you need to cover each of these essential parts.
Essential DAP note components:
- The Data (D) section
Simply put, the Data section is for the data you gather from a session. It can include the significant topics discussed, any interventions used, and how the client responded to these strategies.
Unlike in a SOAP note, all clinician-observed and client-reported symptoms are combined in a DAP note, so you don’t have to spend more time separating out the separate Subjective and Objective sections. - The Assessment (A) section
Once you’ve captured all the important data in the previous section, it’s time to evaluate and assess what all the data means and arrive at a clinical judgement. This is where you can add your clinician’s interpretation, including any diagnoses, or progress made towards treatment goals.
You can also include a re-evaluation of any current interventions being used if they do not seem to be helping the client progress. - The Plan (P) section
Plans the next steps in the client's journey, including what you’d like them to do next and your own goals as their therapist.
This doesn’t need to be the entire treatment plan, but what you’re working toward as part of the therapeutic process.
Need some help? A step-by-step guide
Here’s our head therapist’s step-by-step guide using the DAP acronym.
It’s a neat way to remember what you’re trying to capture in each section.
Benefits of using DAP note templates
Using a progress note template is necessary for legal, insurance, and therapeutic reasons. It can help save time, ensure consistency, and reduce the risk of documentation errors. It also allows for a structured way of writing that is succinct and yet gets to the heart of the client’s journey and progress along their treatment plan.
Specifically, the DAP note structure is commonly used for clinical modalities that are short-term or more driven by solution-focused approaches to therapy.
The DAP format highlights the main problems in one data section which can be faster, and focuses on the practical solutions to solving these problems.
The DAP note also emphasizes comprehensive data collection as the foundation for assessment and planning. Some clinicians consider the DAP note to be more client-focused as a result, and mental health professionals using DAP notes prioritize gathering detailed subjective and objective information to thoroughly understand the client's current state and progress.
DAP notes also offer a more flexible approach to documentation, prioritizing data collection and analysis while allowing therapists to adapt the format to suit individual client needs.
This flexibility enables mental health professionals to tailor their documentation process to the specific requirements of each therapy session, promoting a more personalized approach to client care.
Common use cases for the DAP note template
- Use case no.1
For therapists with a large caseload
DAP notes save time. They’re streamlined and efficient making them useful for therapists who see a high volume of clients. - Use case no.2
For a more client-centered approach to therapy
The DAP progress note template captures the client experience during the session in the Data and Assessment sections. This is helpful for therapists who want to prioritize the client's perspective over a more lengthy analysis as one would see in a SOAP note. - Use case no.3
Situations where discretion is key
Clients may present with severe trauma or other sensitive experiences. To maintain a safe and comfortable therapeutic space, at times, a DAP note is most helpful due to its concise and less intrusive nature. - Use case no.4
Collaborative care settings
Because the DAP note offers a clear and concise summary of the client's progress, it can be beneficial for multidisciplinary team settings with multiple providers.
Additional writing tips for you
Whether you like writing or not, it’s always a good idea to start with a moment of self-care. Being balanced and ready is as much a part of the process for you as it is for your client.
Show up as your best self that day, whatever your limitations. We know that therapists are overworked, but just a few minutes of mindfulness and intentionality can do a lot to free up your mind and create greater focus so you can capture all that you wanted and intended to.
Once you have the mental clarity and space, carefully consider all that you just observed, sensed, and witnessed. Hopefully, you’ll also have given yourself a little time buffer after each session for the note-writing – many therapists leave the documentation to last and then struggle to find the energy and mental clarity they need.
Once you’ve done that, grab your tablet, or paper and pen, and go for it! There’s nothing like diving right in.
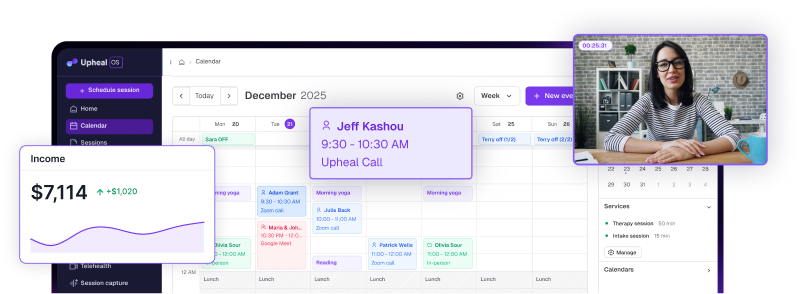
And of course, should you need any help, there are always our trusty AI progress notes – they’ll draft your session notes for you so all you have to do is review and edit. We even offer AI treatment plans.
Concluding thoughts
Ready to write a mental health DAP note now? Hopefully, with the above DAP note example, you feel more confident.
The DAP note is a great choice when dealing with short-term modalities and solution-focused approaches to therapy that allow for more focus on client needs. It’s also a great time-saver!
We hope you liked this article and should you feel that the mental health DAP note isn’t suited to the session you just had or the modality that you’re currently using – feel free to peruse our other article on the use cases for all the progress note types.