A complete guide to SOAP notes (with example)
SOAP Note Example / Template
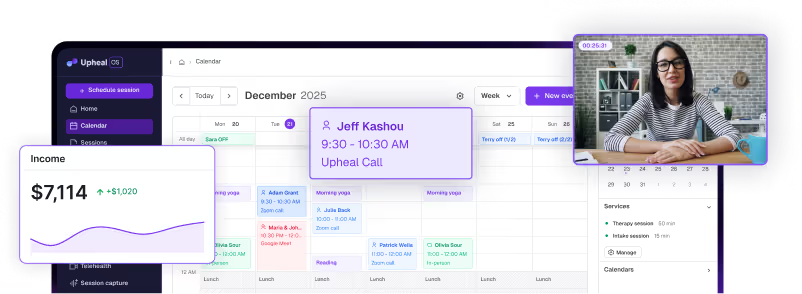
In this guide, you’ll learn what SOAP notes are, how to write effective SOAP therapy notes, and how to use a SOAP note template, including examples of how AI-generated SOAP notes work in practice. We’ll also provide a SOAP note example based on a real-life scenario, and an Upheal template that you can download for free.
What are SOAP notes in therapy?
SOAP notes are a standardized and concise way of capturing data from a client session including what the client is presenting with, their progress, and any future steps toward treatment.
SOAP notes are well-established in healthcare and are used by doctors, psychiatrists, nurses, therapists, psychologists, counselors, social workers, and more, to present a patient’s health findings in a clear and organized manner.
In mental health care, SOAP therapy notes help clinicians clearly document symptoms, progress, and treatment plans, and are increasingly created using AI SOAP note tools. Below is a SOAP note example from a member of our clinical team.
SOAP note therapy example
Here is an example from a real therapy scenario. How would you turn the following session into a mental health SOAP note?
In this case, the contrast between both the physical presentation of depressive symptoms and self-reported emotional experiences will be important to tracking CBT effectiveness and the progress of treatment.
Here is a SOAP note example. It's been written by our Head of Clinical Operations, Ted Faneuff, a licensed therapist, to make sure it's truly helpful to you.
Essential components of a SOAP note
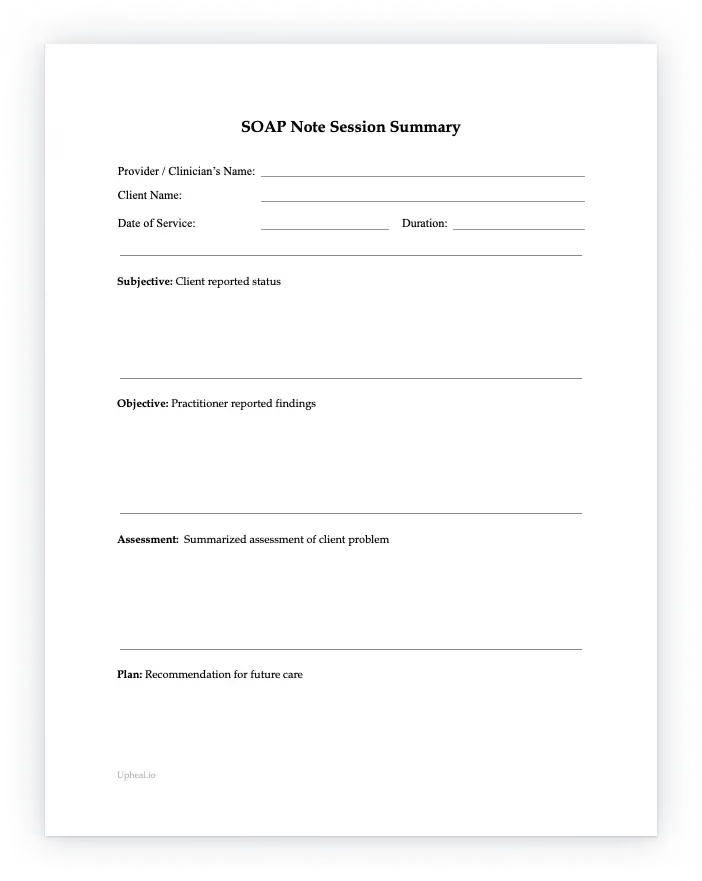
This SOAP note template is designed specifically for therapy SOAP notes and follows the same structure used by AI-generated SOAP notes, making it easy to switch between manual and automated documentation.
As you saw in the SOAP note example, each therapy SOAP note should carefully document the interaction between the client and the therapist and contain the Subjective, Objective, Assessment, and Plan sections.
Healthcare providers can then easily read and understand a client’s history, as can insurance companies.
- Subjective (S): Patient's stated experiences, feelings, and concerns.
- Objective (O): Observable and measurable data collected by the clinician.
- Assessment (A): Clinician's professional judgment and diagnosis.
- Plan (P): Treatment plan, follow-up, and next steps.
Free SOAP note template for therapy (PDF & Word)
Use our free SOAP note template for your clients sessions – it’s free to download.